Welcome to the archives of Wound Care Advisor. Here you have access to a library of original, peer-reviewed, clinical, practical articles from the journal that was published through 2016.
As of January, 2017,Wound Care Advisor is no longer published in traditional journal format – HealthCom Media is now delivering the same high quality, clinical, practical and useful articles, news and practical information, tips and techniques through this website, WoundCareAdvisor.com.
Content on the site is consistently being added and updated – we invite you to bookmark WoundCareAdvisor.com and visit often.
Is there patient care data, such as case studies, short articles or other resources you are interested in sharing with your colleagues? Contact us to learn how you can be a contributor to this site.

2016 Journal: November – December Vol. 5 No. 6
Herpes zoster: Understanding the disease, its treatment, and prevention Herpes zoster (HZ, also called shingles) is a painful condition that produces a maculopapular and vesicular rash. Usually, the rash appears along a single dermatome (band) around one side of the body or face. In most cases, pain, tingling, burning, or itching occurs a few days before the rash. Next, blisters…

2016 Journal: Best of the Best Vol. 5 No. 5
Clinical Notes: Healing SCI Patients, antiseptics on mahout, diabetesElectrical stimulation and pressure ulcer healing in SCI patients A systematic review of eight clinical trials of 517 patients with spinal cord injury (SCI) and at least one pressure ulcer indicates that electrical stimulation increases the healing rate of pressure ulcers. Wounds with electrodes overlaying the wound bed seem to have faster pressureulcer healing than wounds with electrodes placed on intact…

2016 Journal: July – August Vol. 5 No. 4
Practicing emotional intelligence may help reduce lateral violenceIt’s been a stressful day at work—nothing new. One confused patient pulled off her ostomy bag, you’re having difficulties applying negative-pressure wound therapy on another, and a third patient’s family is angry with you. We all experience stressful days, but unfortunately, sometimes we take our stress out on each other. Too often, this ineffective way of identifying and managing stress leads…

2015 Journal: November – December Vol. 4 No. 6
Role of the ostomy specialist clinician in ileal pouch anal anastomosis surgeryRestorative proctocolectomy with ileal pouch anal anastomosis (IPAA) is the gold standard for surgical treatment of ulcerative colitis (UC) or familial adenomatous polyposis (FAP). It’s also done to treat colon and rectal cancers, such as those caused by Lynch syndrome (LS). IPAA allows the patient to maintain fecal continence…
2016 Journal: March – April Vol. 5 No. 2
No more skin tearsImagine watching your skin tear, bleed, and turn purple. Imagine, too, the pain and disfigurement you’d feel.What if you had to live through this experience repeatedly? That’s what many elderly people go through, suffering with skin tears through no fault of their own. Some go on to develop complications.A skin tear is a traumatic wound caused by shear, friction, or blunt-force trauma that results in a…

2016 Journal: January – February Vol. 5 No. 1
Top 10 outpatient reimbursement questionsAt the 2015 Wild on Wounds conference, the interactive workshop “Are You Ready for an Outpatient Reimbursement Challenge?” featured a lively discussion among participants about 25 real-life reimbursement scenarios. Here are the top 10 questions the attendees asked, with the answers I provided.Q Why is it necessary for qualified healthcare professionals (QHPs) such as physicians, podiatrists,…

2016 Journal: May – June Vol. 5 No. 3
How to manage peristomal skin problemsFor an ostomy pouching system to adhere properly, the skin around the stoma must be dry and intact. Otherwise, peristomal skin problems and skin breakdown around the stoma may occur. In fact, these problems are the most common complications of surgical stomas. They can worsen the patient’s pain and discomfort, diminish quality of life, delay rehabilitation, increase use of ostomy supplies, and raise healthcare costs.Peristomal…

2015 Journal: Best of the Best Vol. 4 No. 5
Evolution of the deep tissue injury or a declining pressure ulcer?A declining pressure ulcer decreases the quality of life for patients and places providers at risk for regulatory citations and litigation. But it’s important for clinicians to determine whether the first appearance of skin injury is truly a stage I or II pressure ulcer or if it’s a deep tissue…

2015 Journal: July – Aug Vol. 4 No. 4
Preventing pressure ulcers in pediatric patientsAs wound care clinicians, we are trained—and expected—to help heal wounds in patients of any age and to achieve positive outcomes. Basic wound-healing principles apply to all patients, whatever their age or size. The specific anatomy and physiology of vulnerable pediatric patients, however, requires detailed wound care. Unfortunately, little evidence-based research exists to support and…

2015 Journal: May – June Vol. 4 No. 3
Get the ‘SKINNI’ on reducing pressure ulcersLike many hospitals, Houston Methodist San Jacinto Hospital uses national benchmarks such as the National Database of Nursing Quality Indicators (NDNQI®) to measure quality outcomes. Based on benchmark reports that showed an increased trend of pressure ulcers in critically ill patients in our hospital, the clinical nurses in our Critical Care Shared Governance Unit-Based…

2015 Journal: March – April Vol. 4 No. 2
Palliative wound care: Part 2By preventing and relieving suffering, palliative care improves the quality of life for patients facing problems associated with life-threatening illness. This care approach emphasizes early identification, impeccable assessment, and treatment of pain and other issues—physical, psychosocial, and spiritual.When relieving distressing symptoms takes higher priority than healing the wound, the patient may choose palliative wound care after…

2015 Journal: January – February Vol. 4 No. 1
Healthcare reform and changes provide opportunities for wound care cliniciansQualified healthcare professionals (QHPs), such as physicians, podiatrists, physician assistants, nurse practitioners, and clinical nurse specialists, are taught to diagnose the reasons that chronic wounds aren’t healing and to create plans of care for aggressively managing the wound until it heals. Wound care professionals—nurses and therapists—are taught to implement those plans of…
2014 Journal: November – December Vol. 3 No. 6
Case study: Bariatric patient with serious wounds and multiple complicationsDespite the healthcare team’s best efforts, not all hospitalizations go smoothly. This article describes the case of an obese patient who underwent bariatric surgery. After a 62-day hospital stay, during which a multidisciplinary team collaborated to deliver the best care possible, he died. Although the outcome certainly wasn’t what we wanted,…

2014 Journal: September – October Vol. 3 No. 5
Managing venous stasis ulcersVenous disease, which encompasses all conditions caused by or related to diseased or abnormal veins, affects about 15% of adults. When mild, it rarely poses a problem, but as it worsens, it can become crippling and chronic.Chronic venous disease often is overlooked by primary and cardiovascular care providers, who underestimate its magnitude and impact. Chronic venous insufficiency…
2014 Journal: July August Vol. 3 No. 4
Using maggots in wound care: Part 1Maggot therapy is the controlled, therapeutic application of maggots to a wound. Simple to use, it provides rapid, precise, safe, and powerful debridement. Many wound care professionals don’t provide maggot therapy (also called wound myiasis) because they lack training. But having maggot therapy technology available for patients adds to your capabilities as a wound…
2014 Journal: May – June Vol. 3 No. 3
Understanding therapeutic support surfacesPressure-ulcer prevention and management guidelines recommend support-surface therapy to help prevent and treat pressure ulcers. Support surfaces include pads, mattresses, and cushions that redistribute pressure. Full cushions and cushion pads are considered therapeutic support surfaces if used to redistribute a patient’s pressure in a chair or wheelchair.The National Pressure Ulcer Advisory Panel (NPUAP) defines support surfaces as…

2014 Journal: March April Vol. 3 No. 2
Becoming a wound care diplomatThe Rolling Stones may have said it best when they sang, “You can’t always get what you want,” a sentiment that also applies to wound care. A common frustration among certified wound care clinicians is working with other clinicians who have limited current wound care education and knowledge. This situation worsens when these clinicians are making…

2014 Journal: January February Vol. 3 No. 1
When and how to culture a chronic woundChronic wound infections are a significant healthcare burden, contributing to increased morbidity and mortality, prolonged hospitalization, limb loss, and higher medical costs. What’s more, they pose a potential sepsis risk for patients. For wound care providers, the goal is to eliminate the infection before these consequences arise.Most chronic wounds are colonized by polymicrobial…

2013 Journal: November – December Vol. 2 No. 6
How do you prove a wound was unavoidable?A pressure ulcer that a patient acquires in your facility or a patient’s existing pressure ulcer that worsens puts your organization at risk for regulatory citations as well as litigation. Unless you can prove the pressure ulcer was unavoidable, you could find yourself burdened with citations or fines, or could even end up…
2013 Journal: September – October Vol. 2 No. 5
Developing a cost-effective pressure-ulcer prevention program in an acute-care settingPressure ulcers take a hefty toll in both human and economic terms. They can lengthen patient stays, cause pain and suffering, and increase care costs. The average estimated cost of treating a pressure ulcer is $50,000; this amount may include specialty beds, wound care supplies, nutritional support, and increased staff time…

2013 Journal: July August Vol. 2 No. 4
Understanding stoma complicationsAbout 1 million people in the United States have either temporary or permanent stomas. A stoma is created surgically to divert fecal material or urine in patients with GI or urinary tract diseases or disorders.A stoma has no sensory nerve endings and is insensitive to pain. Yet several complications can affect it, making accurate assessment crucial. These complications…
Top 10 Journal Articles

What you need to know about collagen wound dressings
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS Description Collagen, the protein that gives the skin its tensile strength, plays a key role in each phase of wound healing. It attracts cells, such as fibroblasts and keratinocytes, to the wound, which encourages debridement, angiogenesis, and reepithelialization. In addition, collagen provides a natural scaffold or substrate for new tissue…

Understanding stoma complications
By Rosalyn S. Jordan, RN, BSN, MSc, CWOCN, WCC, OMS; and Judith LaDonna Burns, LPN, WCC, DFC About 1 million people in the United States have either temporary or permanent stomas. A stoma is created surgically to divert fecal material or urine in patients with GI or urinary tract diseases or disorders. A stoma has no sensory nerve endings and…
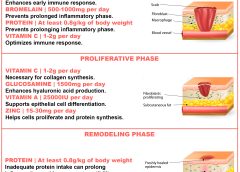
How dietary protein intake promotes wound healing
By Nancy Collins, PhD, RD, LD/N, FAPWCA, and Allison Schnitzer Nutrition is a critical factor in the wound healing process, with adequate protein intake essential to the successful healing of a wound. Patients with both chronic and acute wounds, such as postsurgical wounds or pressure ulcers, require an increased amount of protein to ensure complete and timely healing of their…

Medicare reimbursement for hyperbaric oxygen therapy
By Carrie Carls, BSN, RN, CWOCN, CHRN, and Sherry Clayton, RHIA In an atmosphere of changing reimbursement, it’s important to understand indications and utilization guidelines for healthcare services. Otherwise, facilities won’t receive appropriate reimbursement for provided services. This article focuses on Medicare reimbursement for hyperbaric oxygen therapy (HBOT). (See What is hyperbaric oxygen therapy?) Indications and documentation requirements

What you need to know about hydrogel dressings
By Nancy Morgan, RN, BSN, MBA, WOC, WCC, DWC, OMS Each issue, Apple Bites brings you a tool you can apply in your daily practice. Description Hydrated polymer (hydrogel) dressings, originally developed in the 1950s, contain 90% water in a gel base, which helps regulate fluid exchange from the wound surface. Hydrogel dressing are usually clear or translucent and vary…

Managing venous stasis ulcers
By Kulbir Dhillon, MSN, FNP, APNP, WCC Venous disease, which encompasses all conditions caused by or related to diseased or abnormal veins, affects about 15% of adults. When mild, it rarely poses a problem, but as it worsens, it can become crippling and chronic. Chronic venous disease often is overlooked by primary and cardiovascular care providers, who underestimate its magnitude…
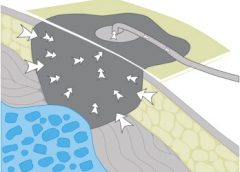
Guidelines for safe negative-pressure wound therapy
By Ron Rock MSN, RN, ACNS-BC Since its introduction almost 20 years ago, negative-pressure wound therapy (NPWT) has become a leading technology in the care and management of acute, chronic, dehisced, traumatic wounds; pressure ulcers; diabetic ulcers; orthopedic trauma; skin flaps; and grafts. NPWT applies controlled suction to a wound using a suction pump that delivers intermittent, continuous, or variable…
The long and short of it: Understanding compression bandaging
By Robyn Bjork, MPT, WCC, CWS, CLT-LANA Margery Smith, age 82, arrives at your wound clinic for treatment of a shallow, painful ulcer on the lateral aspect of her right lower leg. On examination, you notice weeping and redness of both lower legs, 3+ pitting edema, several blisters, and considerable denudement of the periwound skin. She is wearing tennis shoes…

Making sure patients have the ostomy supplies they need
By Connie Johnson, BSN, RN, WCC, LLE, OMS, DAPWCA No matter where you work or who your distributors are, ensuring the patient has sufficient ostomy supplies can be a challenge. Whether you’re the nurse, the physician, the patient, or the family, not having supplies for treatments can heighten frustration with an already challenging situation, such as a new ostomy. Here’s…

Using maggots in wound care: Part 1
By: Ronald A. Sherman, MD; Sharon Mendez, RN, CWS; and Catherine McMillan, BA Maggot therapy is the controlled, therapeutic application of maggots to a wound. Simple to use, it provides rapid, precise, safe, and powerful debridement. Many wound care professionals don’t provide maggot therapy (also called wound myiasis) because they lack training. But having maggot therapy technology available for patients…

